Panacea Journal of Medical Sciences
Panacea Journal of Medical Sciences (PJMS) open access, peer-reviewed triannually journal publishing since 2011 and is published under auspices of the “NKP Salve Institute of Medical Sciences and Research Centre”. With the aim of faster and better dissemination of knowledge, we will be publishing the article ‘Ahead of Print’ immediately on acceptance. In addition, the journal would allow free access (Open Access) to its contents, which is likely to attract more readers and citations to articles published in PJMS.Manuscripts must be prepared in accordance with “Uniform requiremen...

To study correlation between serum uric acid levels and the presence and degree of pre-clinical target organ damage in hypertensive population
Introduction
Worldwide, hypertension is among the leading causes of cardiovascular disease.[1] Its incidence is rising in low-income regions. A few of the effects that high blood pressure may exacerbate include heart failure, coronary heart disease, as well as stroke. [2] As a consequence, a lot of individuals get really sick or pass away. The kidneys and the brain are especially vulnerable to the effects of hypertension. [3] Recognizing Target Organ Damage (TOD) during a hypertensive patient's physical examination might help guide treatment decisions and set goals for blood pressure. It is common for TOD to already be present before hypertension is diagnosed, as is the case in less developed regions. [2], [3] Uric acid elevations are common in hypertensive patients. Due to the link between raised UA levels and a higher risk of cardiovascular disease, the European Society of Hypertension & the European Society of Cardiology both advise routine laboratory testing for serum UA (SUA) in hypertensive patients. [4], [5], [6] Only a few of the cardiovascular risk factors that have been connected to SUA include hypertension, metabolic syndrome, diabetes, and renal disease. It is unclear whether UA is a trustworthy indicator of cardiovascular risk in hypertensive individuals."Multiple large-scale investigations have been done, however UA has not been found to be a significant independent risk factor. [7], [8] The greatest chance of avoiding people with subclinical TOD from developing overt cardiovascular illness is for doctors to recognize them as such. Due to a lack of Echocardiography and Microalbuminuria equipment, screening all newly diagnosed hypertensive patients for subclinical TOD may not be feasible in low-resource settings. UA, which is relatively cheap in comparison to other risk markers, can be used to identify patients at higher risk and guide further evaluation. [9], [10]
Materials and Methods
The study population included both hospitalized and unhospitalized individuals from April 2021 to March 2022 at Rewa, M.P.'s Sanjay Gandhi Hospital and Shyam Shah Medical College. Participants with hypertension ranged in age from 30 to 70 years. The research method used was a ''observational analytical case-control'' approach. In this study there was total number of 200 patients were enrolled out of which 100 hypertensive patients were cases and 100 healthy participants were taken as controls. TOD was defined by the presence of microalbuminuria (urinary albumin excretion: 30-300 mg/d) and Echocardiographic evidence of Left Ventricular Hypertrophy (LVH). Electrocardiographically, the LVH diagnosis was evaluated using - 1) Regardless of gender, Sokolow-Lyon index SV1 + RV5 or V6 ≥35mm was considered LVH.2) According to Cornell's voltage criteria, LVH is defined as SV3 + R aVL> 20 mm in women and > 28 mm in men. 3) Total QRS voltage criteria - Any value ≥175 mm of total QRS voltage was considered as LVH. 4) Romhilt–Estes point Score system (Total Score=12) – [(R or S wave in limb leads ≥ 20 mm OR S V1,V2 or V3 ≥ 25 mm OR R V4,V5 or V6 ≥ 25 mm= 3 points),(ST-T changes= 3 points),(Left atrial involvement-“P” terminal force in V1 > 0.04 sec OR >1mm = 3 points),(Left axis deviation of ≥15°= 2 points),(Intrinsicoid deflection in V5 or V6 ≥0.04 sec = 1 point)]. Any value ≥5 was considered as definite LVH,4 – Probable LVH, and < 4 – no LVH. Only after receiving written informed consent from the patients were routine tests such as ECG and transthoracic echocardiogram, blood pressure check, venous blood sample for Serum Uric Acid (SUA), midstream urine sample for microalbuminuria (patients with proteinuria on dipstick testing will be included), and routine tests performed (serum creatinine, fasting lipid profile, and plasma glucose).
Inclusion criteria
All adults new cases of Hypertension.
Exclusion criteria
Patients taking medications that are known to alter uric acid levels in the blood, such as diuretics, ACE inhibitors, or ARBs.
Ethical clearance
After being made aware of the study's objectives and providing written informed permission that was sanctioned by the institutional ethics committee, all patients and their families took part in it.
Statistical analysis
With the use of the statistical programme SPSS 20.0, the data were evaluated after being entered into a Microsoft Excel spreadsheet. Data was presented using mean ±SD. Quantitative data analysis: To determine the significance of the event ANOVA tests were used.
Results
Discussion
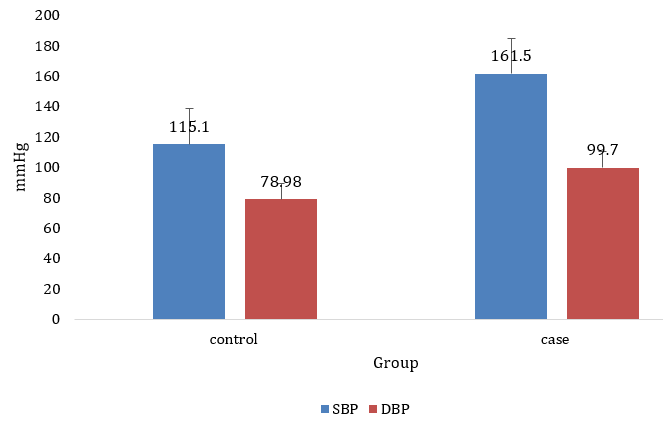
In this study, patients mean (standard deviation) diastolic and SBP were 161.5 ±17.73 and 99.7 ±9.53, compared to 115.1 ±5.806 for controls.
Cases had a mean and SD of 5.39±1.26 for Sr. Uric Acid, whereas controls had a mean and SD of 3.97± 0.61; this disparity is indicative of a substantial effect of Systemic Hypertension severity on Sr. Uric Acid level (P <0.001).
Almost same findings were found in studies by KothiaDivyen et al., [9] Piani F. et al., [10] and Ofori SN. et al. [11] These studies show aassociation between the SUA levels of hypertensive and normotensive individuals & a connection between the SUA levels and the duration and severity of hypertension.
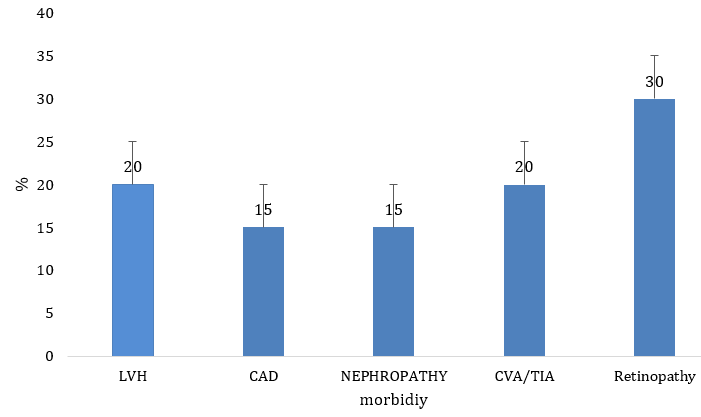
Among the hypertensive people in our research, 20% (N= 20) had LVH. In cases with LVH, serum uric acid levels averaged 5.92±1.39 mg/dL, but in those without the disease, they averaged 4.67±1.18 mg/dL (P<0.001). The occurrence of hypertension in hypertensives with CAD was 15% (N= 15). Patients with CAD had a mean Sr. uric acid level of 5.71±1.23, whereas those without CAD had a level of 4.61±1.19 (P< 0.001). 12.0 percent of hypertensive people (N=12) had nephropathy. The typical level of serum uric acid in people with kidney failure was 5.831±1.29, which was substantially higher than the 4.73±1.23 level observed in healthy individuals (P< 0.001). Among people with hypertension, a stroke or TIA occurred in 20% (N=20) of cases. Patients with CVA/TIA had a mean Sr Uric Acid of 5.31±1.55, while those without CVA/TIA had a mean of 4.75±1.22. Hypertensives had an incidence of retinopathy of 30% (N=30). Patients diagnosed with retinopathy had significantly higher sr. uric acid levels (5.81±1.32) compared to those without the condition (4.46±1.06) (P<0.001). When comparing instances with and without LVA, CAD, NEPHROPATHY, CVA, and Hypertensive Retinopathy, a statistically significant difference was found (P< 0.001).
Microalbuminuria was more prevalent in patients with hypertension and hyperuricemia (54.1%) than it was in those with normal uric acid levels (24.6%) (P = 0.001). Similar to the previous example, those with high blood pressure and elevated uric acid levels had a higher risk of left ventricular hypertrophy than those with the same blood pressure but normal uric acid levels (70.5 vs. 42.0, respectively; P=0.001). Whether no organs were affected, one was injured, or both were injured led to a linear increase in uric acid levels (P=0.012). The target organs of hypertensives were shown to have more severe damage when serum uric acid levels were high. The results of the previous study are supported by our research.
The serum uric acid levels of patients with target organ damage were considerably greater than those of patients with normal blood uric acid levels (Viazzi F et al.,). [12] This was true regardless of whether the patients had left ventricular hypertrophy, carotid abnormalities, microalbuminuria, or any other form of organ damage. Our results were consistent with those of previous research by Viazzi F et al. According to data collected for the PAMELA project, a rise in SUA is a risk factor for the emergence of hypertension and Left Ventricular Hypertrophy in the general population (conducted in part by Grassi G et al 76).
According to a cross-sectional study by Zhang X et al., [13] patients with LVH had an SUA of 0.41 (95 percent confidence interval: 0.28–0.53), which was noticeably higher than the SUA of patients without LVH. The findings of Kumar M. et al. [14] were consistent with these in terms of Target Organ Damage". Hyperuricemia is linked to left ventricular hypertrophy (x2=23.97, p<0.0001), as shown in a study by Fasae AJ et al. [15]
Conclusion
In summary, our work demonstrates that elevated SUA in a sample of untreated patients with primary hypertension is a sign of subclinical TOD. These findings indicate SUA's potential relevance as a flexible, independent marker of TOD.
To determine whether SUA reduction in and of itself imparts cardiovascular protection and the potential function it may play as a surrogate end point of antihypertensive medication, more research is required.
Patients with hypertension have mean serum uric acid concentrations that are unrelated to BMI, blood sugar, or renal markers such as blood urea or serum creatinine. When compared to normotensives, hypertensives have greater serum uric acid levels. This biochemical marker can be used to gauge the severity of hypertension at an early stage since blood uric acid increased more in long-term hypertensives than in short-term hypertensives. In newly diagnosed hypertensive individuals as opposed to pre-hypertensive patients, serum uric acid was more strongly linked with the severity of the hypertension. Studies on the impact of reducing serum uric acid levels in the management of hypertension have led to the conclusion that early detection and management of hypertension may be feasible if medical professionals are more vigilant in tracking their patients' blood pressure.
Research on the connection between hypertension and end-organ damage due to elevated uric acid levels in the blood is warranted.
Source of Funding
No funding sources.
Conflict of Interest
None.
Ethical Approval
The study was approved by the institutional ethics committee.
References
- AV Chobanian, GL Bakris, HR Black, WC Cushman, LA Green, JL Izzo. 1.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo Jr JL, Jones DW, Materson BJ, Oparil S, Wright Jr JT, Roccella EJ. Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. hypertension. 2003 Dec 1;42(6):1206-52.. Hypertension 2003. [Google Scholar]
- JA Whitworth. 2003 World Health Organization (WHO)/International Society of Hypertension (ISH) statement on management of hypertension. J Hypertens 2003. [Google Scholar]
- F Eric, M Marco. The Links between academic research and public policies in the field of migration and ethnic relations: selected national case studies; thematic introduction. Int J Multicultural Soc 2005. [Google Scholar]
- BL Salako, OS Ogah, AA Adebiyi, KS Adedapo, CO Bekibele, TS Oluleye. Unexpectedly high prevalence of target-organ damage in newly diagnosed Nigerians with hypertension. Cardiovasc J Afr 2007. [Google Scholar]
- PJ Cannon, WB Stason, FE Demartini, SC Sommers, JH Laragh. Hyperuricemia in primary and renal hypertension. N Engl J Med 1966. [Google Scholar]
- . European Society of Hypertension-European Society of Cardiology Guidelines Committee. 2003 European Society of Hypertension-European Society of Cardiology guidelines for the management of arterial hypertension. J Hypertens 2003. [Google Scholar]
- BF Culleton, MG Larson, WB Kannel, D Levy. Serum uric acid and risk for cardiovascular disease and death: the Framingham Heart Study. Ann Intern Med 1999. [Google Scholar]
- WB Duffy, HO Senekjian, TF Knight, EJ Weinman. Management of asymptomatic hyperuricemia. JAMA 1981. [Google Scholar]
- K Divyen, SC Aundhakar, NL Sutariya, R Vartika, P Hardik. Evaluation of roleserum uric acid levels in cases of essential hypertension. Intl J Contemp Med Res 2018. [Google Scholar]
- F Piani, AF Cicero, C Borghi. Uric Acid and Hypertension: Prognostic Role and Guide for Treatment. J Clin Med 2021. [Google Scholar] [Crossref]
- SN Ofori, OJ Odia. Serum uric acid and target organ damage in essential hypertension. Vasc Health Risk Manag 2014. [Google Scholar] [Crossref]
- F Viazzi, D Parodi, G Leoncini, A Parodi, V Falqui, E Ratto. Serum uric acid and target organ damage in primary hypertension. Hypertension 2005. [Google Scholar]
- X Zhang, R Yuan, H Ding, X Han, J Yu. A2808 Association between serum uric acid and left ventricular hypertrophy in essential hypertension: A meta-analysis. J Hypertens 2018. [Google Scholar] [Crossref]
- M Kumar, D Prasad, P Yugal, D Jana. Serum Uric Acid and Target Organ Damage In Essential Hypertension At Medicine Department of Gmc. Int J Scientific Res 2020. [Google Scholar]
- AJ Fasae, OA Busari, R Oluyombo, M Yusuf, OG Opadijo, AB Omotoso. Hyperuricemia and Its Correlation with Target Organ Damage and Electrocardiographic Changes in Newly Diagnosed Adult Nigerian Hypertensive Patients. Clin Med Res 2018. [Google Scholar]
Article Metrics
- Visibility 6 Views
- Downloads 3 Views
- DOI 10.18231/j.pjms.2024.141
-
CrossMark
- Citation
- Received Date March 28, 2023
- Accepted Date August 08, 2023
- Publication Date December 21, 2024