Panacea Journal of Medical Sciences
Panacea Journal of Medical Sciences (PJMS) open access, peer-reviewed triannually journal publishing since 2011 and is published under auspices of the “NKP Salve Institute of Medical Sciences and Research Centre”. With the aim of faster and better dissemination of knowledge, we will be publishing the article ‘Ahead of Print’ immediately on acceptance. In addition, the journal would allow free access (Open Access) to its contents, which is likely to attract more readers and citations to articles published in PJMS.Manuscripts must be prepared in accordance with “Uniform requiremen...

Diagnostic utility of neutrophil to lymphocyte ratio in adult population of type 2 diabetes mellitus: A tertiary care centre experience
Introduction
Diabetes mellitus is a metabolic condition characterized by impaired glucose tolerance and peripheral insulin resistance. It is one of the major causes of increased mortality and morbidity with microvascular and macrovascular complications.[1] According to the International Diabetes Federation in 2019, the worldwide prevalence of diabetes mellitus has increased drastically from 30 million cases in 1985 to 463 million in 2019. 1 in 11 adults aged 20-79 years is having diabetes. According to the latest study, it is also estimated that there will be around 642 million cases of diabetes by the year 2040.[2], [3] Systemic inflammation plays a vital role in insulin resistance and type 2 diabetes mellitus.[4] Several studies have been done that suggest that levels of various inflammatory markers are raised in diabetes mellitus and are associated with an increased risk of cardiovascular disease and complications.[5], [6], [7] Neutrophil to lymphocyte ratio (NLR) is a hemogram-derived simple marker that can be used to assess underlying inflammation and diabetic control levels.[8], [9] We compared NLR and Glycated hemoglobin A (HbA1c) levels in diabetic patients and healthy controls to establish a possible correlation between NLR and HbA1c levels.
Materials and Methods
This was a case-control study, including 100 cases of type 2 diabetes mellitus and similar age & sex-matched healthy controls. Consent was obtained from each participant of the study. Cases of type 2 diabetes mellitus aged between 18 to 60 years were taken based on the American Diabetes Association (ADA) 2020 criteria.[10] Any cases with active or chronic disease, history of recent infections, type 2 diabetes mellitus patients taking treatment, and patients of type 1 diabetes mellitus were excluded from the study. 2 ml of venous blood was taken in a sterile vial containing anticoagulant Ethylenediaminetetraacetic acid. The sample was run on a 5-part differential counter analyzer. A differential count was obtained and NLR was calculated by dividing absolute neutrophil count by absolute lymphocyte count. The samples were also run on a Hemo one machine for HbA1c estimation. Statistical analysis was done by using the Statistical Package for the Social Sciences licensed version 21.0. After calculating the mean and standard deviation (SD), a paired t-test was applied for quantitative data. A p-value ≤ 0.05 was considered statistically significant.
Results
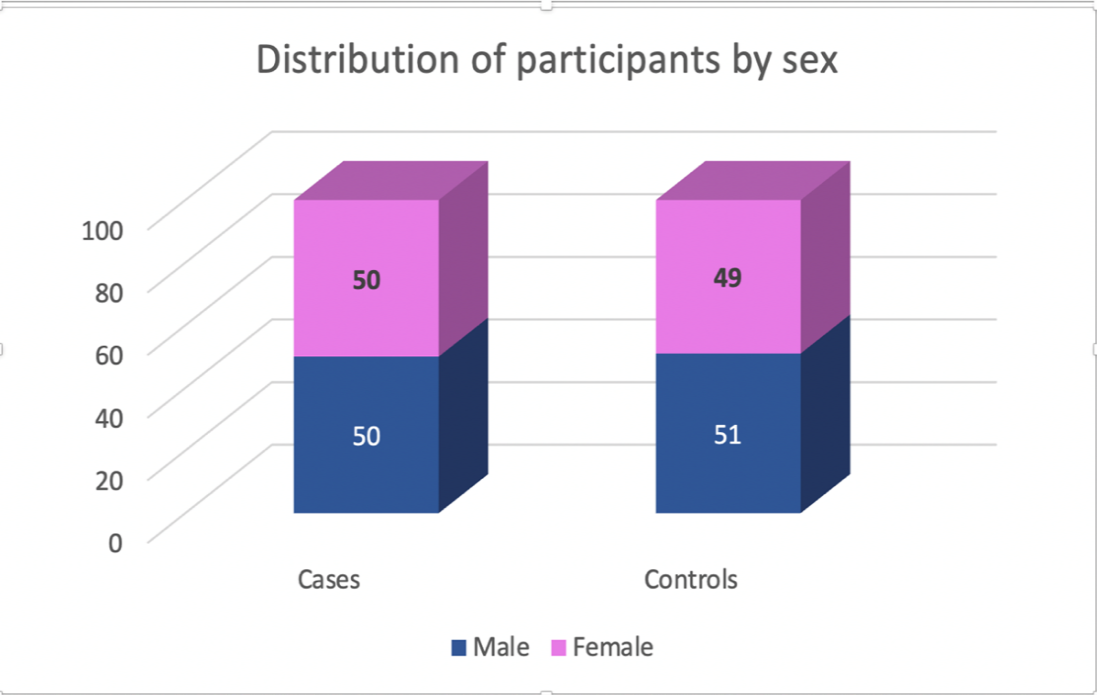
In this study, 100 type 2 diabetes mellitus patients (50.0%) were taken as cases and 100 (50.0%) healthy individuals were taken as controls. The mean (SD) of age (years) in the cases was 46.45 (8.01) and in the controls was 45.6 (8.05). The age (years) in the cases ranged from 30 to 60 and in the controls ranged from 31 to 60 ([Table 1]). 50% of the participants in the cases were males and 50% were females in the cases group. 51% were male and 49% were females in the control group ([Figure 1]). Cases and controls were age and sex-matched. No significant difference was seen among the cases and control groups in terms of age and sex (p > 0.05).
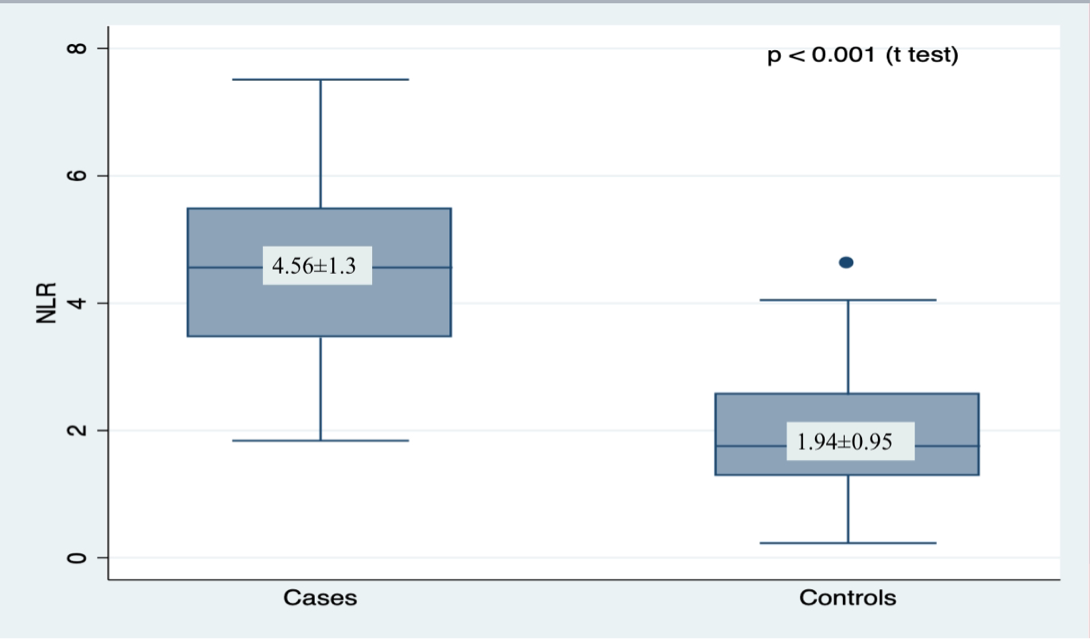
The mean (SD) value of NLR in the cases group was 4.56 (1.3) and in the control was 1.94 (0.95). The distribution of NLR in the cases and controls is depicted by the Box-and-Whisker plot. The upper and lower extent of the whiskers represent the Tukey limits for NLR in each of the groups while the upper and lower boundaries of the box represent the 75th and the 25th centile of NLR respectively and the middle horizontal line represents the median NLR ([Figure 2]). Results were calculated using a t-test, the mean NLR in patients with type 2 diabetes mellitus was compared with the mean NLR of healthy controls and found to be significantly elevated (p<0.001).
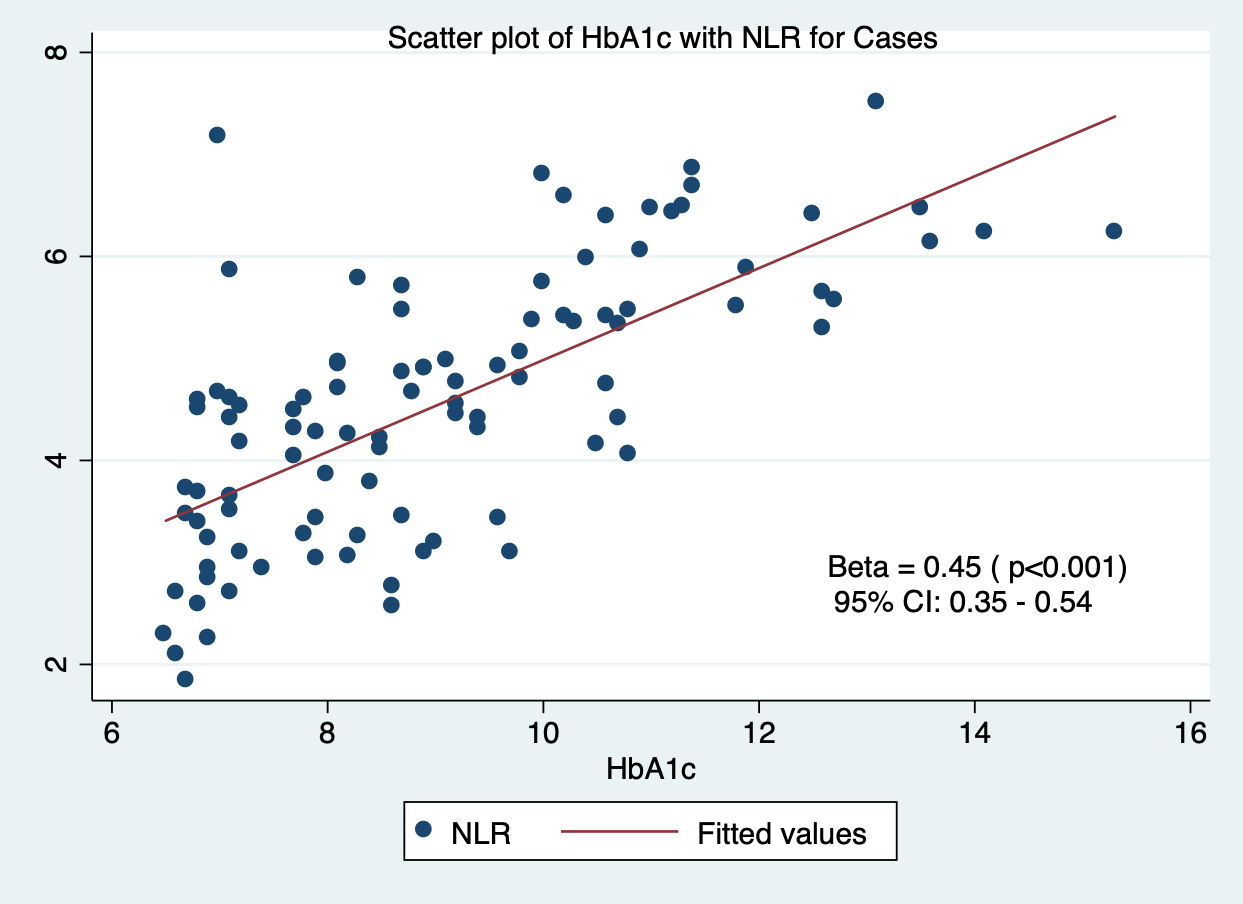
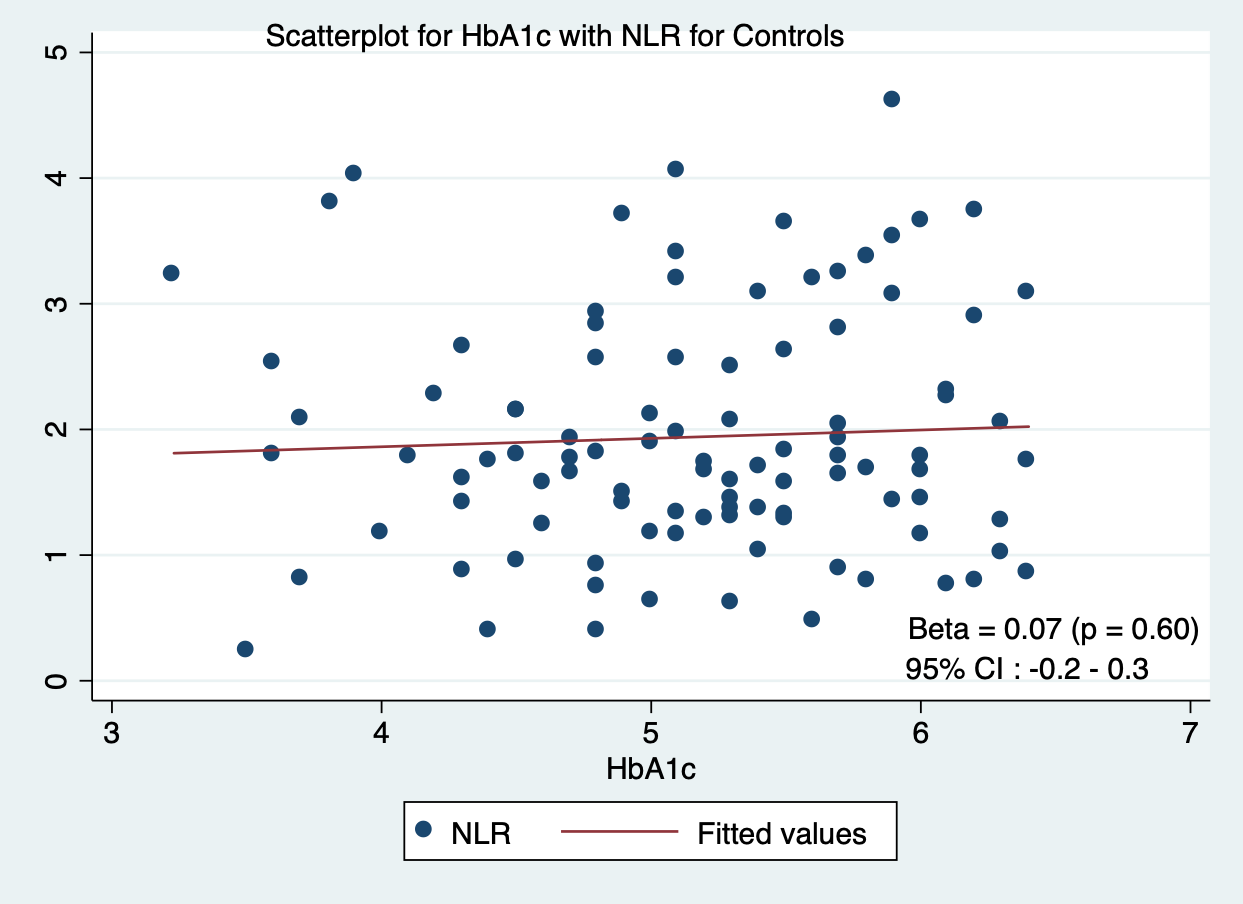
The correlation between NLR and HbA1c is depicted by scatterplot. The red line shows the general trend of correlation between the two variables and individual points represent individual cases. We found a significant positive correlation between NLR and HbA1c levels in type 2 diabetes mellitus patients (p-value ≤ 0.05) ([Figure 3]), while no correlation was seen between NLR and HbA1c levels in healthy controls ([Figure 4]).
|
|
Mean age |
Std. Deviation |
Minimum |
Maximum |
|
Cases |
46.45 |
8.01 |
30 |
60 |
|
Controls |
45.6 |
8.05 |
31 |
60 |
Discussion
The present study showed that the value of NLR is higher in cases of type 2 diabetic patients when compared to healthy controls. Also, NLR values are positively correlated with HbA1c values. It suggested a possible role of NLR as a novel marker in measuring diabetic control levels. Sefil F et al.[11] conducted a retrospective study and found that white blood cell counts, neutrophils, and fasting serum glucose were significantly higher in the diabetic group. Also, a positive correlation was observed between NLR and HbA1c. Similarly, in a study conducted by Duman TT et al.,[12] higher values of NLR were suggestive of diabetic control levels in type 2 diabetes mellitus cases. It was also found that NLR was positively correlated with fasting glucose levels and HbA1c. Various studies have already suggested a crucial role of inflammation in the pathogenesis of diabetes mellitus and metabolic syndrome. [13], [14], [15], [16], [17] Umarani et al. studied the relationship between NLR with different levels of glucose intolerance. It was found that NLR was increased in cases of complicated diabetes mellitus as compared to the cases with diabetes mellitus under control. Hence, it was established that NLR can be used as an early prognostic marker in patients with diabetes mellitus for microvascular complications.[18] Liu et al. also conducted a study to find an association between NLR and type 2 diabetes mellitus patients with peripheral neuropathy. It was suggested that patients of type 2 diabetes mellitus with higher NLR levels might be more likely to develop peripheral neuropathy complications. [19] Qiao S et al. documented that a higher value of NLR had an independent prognostic role in patients with both type 2 diabetes mellitus and coronary artery diseases. [20]
Rahar S et al. revealed higher NLR in cases of diabetic patients when compared to controls. A significantly higher value of NLR was found in cases of diabetic nephropathy as compared to the diabetic cases with normal renal function group and control group.[21] Researchers have also found significantly increased NLR value and platelet-to-lymphocyte ratio in diabetic nephropathy cases. Their role as a prognostic and predictor marker in cases of diabetic nephropathy was suggested.[22] In a retrospective study, a higher NLR value in cases of uncontrolled type 2 diabetes mellitus was found as compared to cases of controlled type 2 diabetes mellitus, but it was statistically insignificant.[23]
Conclusion
There is very limited literature available regarding the correlation of NLR with HbA1c levels in patients with type 2 diabetes mellitus. Elevated value of NLR in healthy individuals may be indicative of underlying chronic low-grade inflammation and impaired glucose metabolism. NLR is a simple parameter that can be used as a valuable tool to monitor diabetic control levels along with HbA1c in type 2 diabetic subjects. Underlying inflammation can also be assessed at the subliminal stage, hence, morbidity and mortality related to microvascular and macrovascular complications can be reduced with an early intervention.
Source of Funding
None.
Conflict of Interest
None.
References
- N Nakhro, P Khambra, S Sharma, TB Singha. Metabolic consequences on platelet parameters: Mean platelet volume and platelet distribution width in type 2 diabetes mellitus. Asian J Med Sci 2024. [Google Scholar]
- Y Zheng, SH Ley, FB Hu. Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat Rev Endocrinol 2018. [Google Scholar]
- P Saeedi, I Petersohn, P Salpea, B Malanda, S Karuranga, N Unwin. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract 2019. [Google Scholar]
- S Tsalamandris, AS Antonopoulos, E Oikonomou, GA Papamikroulis, G Vogiatzi, S Papaioannou. The Role of Inflammation in Diabetes: Current Concepts and Future Perspectives. Eur Cardiol 2019. [Google Scholar]
- IM Taha, AM Abdulla, H Elimam. Inflammatory markers and control of type 2 diabetes mellitus. Diabetes Metab Syndr 2019. [Google Scholar]
- A Pfutzner, T Schondorf, M Hanefeld, T Forst. High Sensitivity C-Reactive Protein predicts cardiovascular risk in diabetic and nondiabetic patients. J Diabetes Sci Technol 2010. [Google Scholar]
- S Raj, G V Rajan. Correlation between elevated serum ferritin and HbA1c in type 2 diabetes mellitus. Int J Res Med Sci 2013. [Google Scholar]
- A Shiny, YS Bibin, CS Shanthirani, BS Regin, RA Anjana, M Balasubramanyam. Association of neutrophil-lymphocyte ratio with glucose intolerance- an indicator of systemic inflammation in patients with type 2 diabetes. Diabetes Technol Ther 2014. [Google Scholar]
- P Forget, C Khalifa, JP Defour, D Latinne, MC Van Pel, MD Kock. What is the normal value of the neutrophil-to-lymphocyte ratio?. BMC Res Notes 2017. [Google Scholar]
- . American Diabetes Association. 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2020. Diabetes Care 2020. [Google Scholar]
- F Sefil, K T Ulutas, R Dokuyucu, A T Sumbul, E Yengil, AE Yagiz. Investigation of neutrophil-lymphocyte ratio and blood glucose regulation in patients with type 2 diabetes mellitus. J Int Med Res 2014. [Google Scholar]
- TT Duman, G Aktas, BM Atak, MZ Kocak, E Erkus, H Savli. Neutrophil to lymphocyte ratio as an indicative of diabetic control level in type 2 diabetes mellitus. Afr Health Sci 2019. [Google Scholar]
- T Reinehr, CL Roth. Inflammation Markers in Type 2 Diabetes and the Metabolic Syndrome in the Pediatric Population. Curr Diab Rep 2018. [Google Scholar]
- SM Haffner. The metabolic syndrome: inflammation, diabetes mellitus, and cardiovascular disease. Am J Cardiol 2006. [Google Scholar]
- A Mankowska, J Pollak, G Sypniewska. Association of C- Reactive Protein and Other Markers of Inflammation with Risk of Complications in Diabetic Subjects. EJIFCC 2006. [Google Scholar]
- A Brahimaj, S Ligthart, M Ghanbari, MA Ikram, A Hofman, OH Franco. Novel inflammatory markers for incident pre-diabetes and type 2 diabetes: the Rotterdam Study. Eur J Epidemiol 2017. [Google Scholar]
- NG Forouhi, AH Harding, M Allison, MS Sandhu, A Welch, R Luben. Elevated serum ferritin levels predict new-onset type 2 diabetes: results from the EPIC- Norfolk prospective study. Diabetologia 2007. [Google Scholar]
- MK Umarani, K Sahi, M Bharathi. Study of Neutrophil-Lymphocyte ratio (NLR) in diabetes mellitus. Trop J Pathol Microbiol 2020. [Google Scholar]
- S Liu, H Zheng, X Zhu, F Mao, S Zhang, H Shi. Neutrophil-to-lymphocyte ratio is associated with diabetic peripheral neuropathy in type 2 diabetes patients. Diabetes Res Clin Pract 2017. [Google Scholar]
- S Qiao, W Gao, S Guo. Neutrophil-Lymphocyte Ratio (NLR) for Predicting Clinical Outcomes in Patients with Coronary Artery Disease and Type 2 Diabetes Mellitus: A Propensity Score Matching Analysis. Ther Clin Risk Manag 2020. [Google Scholar]
- S Rahar, S Marwah, B Kulshreshtha. Neutrophil lymphocyte ratio (NLR) in type 2 diabetes mellitus and its correlation with renal function: An institutional experience. J Dr. NTR Univ Health Sci 2021. [Google Scholar]
- M Jaaban, AB Zetoune, S Hesenow, R Hessenow. Neutrophil-lymphocyte ratio and platelet-lymphocyte ratio as novel risk markers for diabetic nephropathy in patients with type 2 diabetes. Heliyon 2021. [Google Scholar]
- H Ozisik, S Cetinkalp, A Suner, G Ozgen, F Saygili, M Erdogen. The relationship between neutrophil lymphocyte ratio and diabetes control in patients with type 2 diabetes mellitus. Ege Tıp Dergisi 2022. [Google Scholar]
Article Metrics
- Visibility 6 Views
- Downloads 3 Views
- DOI 10.18231/j.pjms.2024.148
-
CrossMark
- Citation
- Received Date September 23, 2023
- Accepted Date March 20, 2024
- Publication Date December 21, 2024