Panacea Journal of Medical Sciences
Panacea Journal of Medical Sciences (PJMS) open access, peer-reviewed triannually journal publishing since 2011 and is published under auspices of the “NKP Salve Institute of Medical Sciences and Research Centre”. With the aim of faster and better dissemination of knowledge, we will be publishing the article ‘Ahead of Print’ immediately on acceptance. In addition, the journal would allow free access (Open Access) to its contents, which is likely to attract more readers and citations to articles published in PJMS.Manuscripts must be prepared in accordance with “Uniform requiremen...

A case series of right sided infective endocarditis (IE) in a tertiary care hospital
Introduction
Infective endocarditis is characterized by infection of heart valves or intracardiac devices.IE can present rapidly (acute IE) or insidiously (subacute IE) over days to weeks. IE must always be a differential in anyone presenting with prolonged fever, weight loss and malaise irrespective of murmurs. Mortality rates may range upto 25 % even with appropriate treatment.[1] Absence of overemphasized classic signs of Osler’s nodes or Janeway lesions does not rule out IE.[2] The incidence of IE in North America and Western Europe is 1.7 – 6.2 per 100,000 person-years. Rheumatic heart disease was the most common lesion in the past, and the mitral valve was most commonly involved site in developing countries but the picture is different in developed countries.[3] Prosthetic valves and cardiac devices (permanent pacemakers and ICDs) are also risk factors for IE. Congenital heart disease also cause increased risk of IE. The common causative organisms include streptococci, staphylococci, enterococci, fastidious organisms, gram negatives and fungi. Organism can be predicted as per clinical presentation like Staphylococcus epidermidis in early prosthetic valve endocarditis and blind antibiotic treatments can be planned pending culture and sensitivity reports. [4]
Materials and Methods
The present study was a retrospective study from the year 2018 of all infective endocarditis patients admitted in our medical units at our hospital diagnosed based on symptoms, blood culture reports and echocardiography reports. None of the three patients had features suggestive of splinter haemorrhages and osler’s nodes .
Case Series
The pattern of illness, hallmark features and echocardiography reports are highlighted here.
Case 1
A 36 years old married lady known case of SLE on 7.5 mg prednisolone was admitted to a nursing home with dengue and was treated conservatively. Subsequently the lady was admitted to our hospital few weeks later with rash over peripheral cannulation site (done at previous hospital over saphenous vein of right lower limb possibly due to inaccessible upper limb veins), high grade fever and dyspnea.([Figure 1]). On examination she was febrile, tachypneic and had left pleural effusion.([Figure 2]) Thoracentesis revealed exudative neutrophilic high protein pleural fluid. No murmur was heard. Laboratory reports revealed neutrophilic leukocytosis (TC 12,500, neutrophil 82%, lymphocyte 14%, eosinophil 1%, monocyte 3% and basophil 0%). Blood culture grew Staphylococcus aureus sensitive to vancomycin. In view of above findings transthoracic echocardiography was done which revealed vegetation over tricuspid valve.([Figure 3]) Patient was treated with Inj Vancomycin for 6 weeks with intercostal drainage of left pleural effusion and she recovered.


Case 2
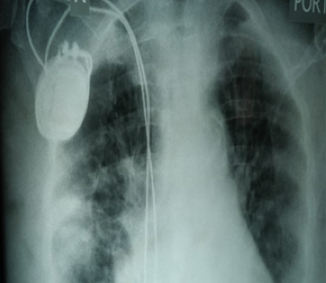
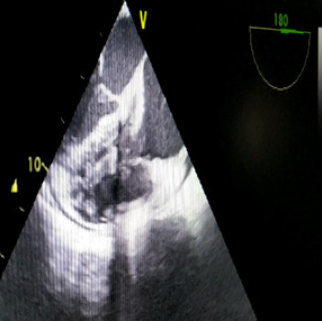
A 76 years old lady known diabetic presented with anasarca but denied any history of fever. On examination she had features of right heart failure with elevated jugular venous pressure, pedal edema, ascites and tender hepatomegaly. No murmur was heard. She had a permanent pacemaker implanted two years earlier. Laboratory reports revealed neutrophilic leukocytosis (TC 30,500/cu.mm, neutrophil 90%, lymphocyte 5%, eosinophil 1%, monocyte 4% and basophil 0%), active urinary sediment with 25-26 pus cells/hpf, red cells 5-6/hpf and trace albumin. Blood culture did not grew any organism. Chest X ray revealed infiltrates involving right lung with pacemaker in situ.([Figure 4]) Transesophageal echocardiography revealed large vegetation on pacemaker lead which was missed on transthoracic echocardiography. ([Figure 5]) Patient was put on Inj Vancomycin and gentamicin but succumbed to the illness before we could proceed for surgical correction.
Case 3
A 31 years old male known case of aplastic anaemia on regular blood transfusions as and when needed but not on any immunosuppressives presented with on and off fever and malaise along with weight loss. He had mild pedal edema. On examination he had a pansystolic murmur over tricuspid area. Complete hemogram revealed pancytopenia (TC 2200 / cu.mm, neutrophil 12 %, lymphocyte 84%, eosinophil 1%, monocyte 3%, basophil 0 %, hemoglobin 8.6 gm/dl, platelet 44,000/cu.mm). Blood culture grew Enterococcus faecalis which was resistant to vancomycin. Transthoracic echocardiography showed vegetation over tricuspid valve. ([Figure 6]) The patient has been put on Inj Ampicillin and Ceftriaxone and is still to complete his 6 weeks of therapy but his inflammatory markers like ESR and CRP have come down and he is improving clinically.
Discussion
Right-sided native valve infective endocarditis involves the tricuspid or pulmonary valve. Isolated right heart IE accounts for approximately 10 percent of all IE cases; concomitant left-sided and right-sided IE account for approximately 13 percent of all IE cases. [5] Risk factors include injection drug use, presence of a cardiac implantable device, infected vascular catheters and presence of an right-sided cardiac anomaly.
Right-sided infective endocarditis approximates for 5-10% of all cases of infective endocarditis, and is encountered in IV drug abuser, where HIV and HCV coinfections may coexist. Staphylococcus aureus is the most common pathogen. The disease usually presents as a persistent fever with respiratory symptoms without signs of systemic embolisation as seen in left-sided IE. The diagnosis requires a high index of suspicion. Transthoracic echocardiography can diagnose, whilst transesophageal echocardiography can increase sensitivity. Virulence of the causative organism and vegetation size are the major determinants of prognosis. Most cases recover with appropriate antibiotics. [6]
The diagnostic algorithm for patients with suspected IE includes fever with respiratory symptoms, blood cultures (at least three sets obtained from separate venipuncture sites prior to initiation of antibiotics) electrocardiography, chest radiography and echocardiography.
The unique nature of illnesses in our cases include acuteness of presentation in case 1 and subacute nature in case 2 and 3. Case 1 was due to infected peripheral venous catheter site with haematogenous dissemination of Staphylococcus aureus with background SLE on low dose steroids. This highlights the importance of asepsis during catheter placement and inspection of vascular catheters on ward rounds and prompt removal if any signs of inflammation and treat if required if catheter related blood stream infection is suspected to avoid similar future complications. Also people on steroid for long term should have minimal handling of vascular catheters as health care workers are a major source of contamination. Handwashing importance is also very important. [7] Case 2 was pacemaker lead endocarditis but we could not isolate any organism. This case highlights the fact that any patient with pacemaker or any foreign device if presents with long standing undiagnosed fever, malaise, weight loss should be evaluated for endovascular infections. Also mortality is higher in case of device infections. [8] Case 3 involves an immunocompromised patient with possible venous source of Enterococcus faecalis during any of his blood transfusion sessions. This case highlights the importance of maintaining a high degree of asepsis in patients on recurrent blood transfusion regime and to investigate appropriately if those patients presents with subacute illness like fever and fatigue. None of the patients had osler’s nodes and splinter haemorrhages highlighting the importance of suspecting IE even in their absence.
Conclusion
The cases are presented due to their rarity and uniqueness of presentation. The hallmarks include importance of handwashing before procedures, maintain strict care of vascular catheters and prompt action on suspicion of endovascular infection due to catheters or devices.
Source of Funding
None.
Conflict of Interest
None.
References
- DR Murdoch, GR Corey, B Hoen, JM Miró, VG Fowler Jr, AS Bayer. Clinical presentation, etiology, and outcome of infective endocarditis in the 21st century: the International Collaboration on Endocarditis-Prospective Cohort Study. Arch Intern Med 2009. [Google Scholar]
- NJ Gross, R Tall. Clinical significance of splinter haemorrhages. Br Med J 1963. [Google Scholar]
- S Rabinovich, J Evans, IM Smith, LE January. A Long-Term View of Bacterial Endocarditis. 337 Cases 1924 to 1963. Ann Intern Med 1965. [Google Scholar] [Crossref]
- VG Fowler, JM Miro, B Hoen, CH Cabell, E Abrutyn, E Rubinstein. Staphylococcus aureus endocarditis: a consequence of medical progress. JAMA 2005. [Google Scholar]
- J Chahoud, A Sharif Yakan, H Saad, SS Kanj. Right-Sided Infective Endocarditis and Pulmonary Infiltrates: An Update. Cardiol Rev 2016. [Google Scholar]
- K Akinosoglou, E Apostolakis, M Marangos, G Pasvol. Native valve right sided infective endocarditis. Eur J Intern Med 2013. [Google Scholar]
- D Pittet, B Allegranzi, H Sax, S Dharan, CL Pessoa-Silva, L Donaldson. Evidence-based model for hand transmission during patient care and the role of improved practices. Lancet Infect Dis 2006. [Google Scholar]
- IS Schwartz, N Pervez. Bacterial endocarditis associated with a permanent transvenous cardiac pacemaker. JAMA 1971. [Google Scholar]
Article Metrics
- Visibility 6 Views
- Downloads 3 Views
- DOI 10.18231/j.pjms.2024.163
-
CrossMark
- Citation
- Received Date March 09, 2022
- Accepted Date December 05, 2022
- Publication Date December 21, 2024